Depression is a serious mental illness that impacts millions of people worldwide. If you’re struggling with depression, it’s essential to understand the various treatment options available.
Depression, frequently referred to as clinical depression or major depressive disorder, is a mood disorder marked by a loss of interest in activities, persistent sadness, and hopelessness. People suffering from this mental condition may have trouble performing even the most basic of daily tasks, and at times they may question whether or not they should continue living.
According to the 2020 data published by SAMHSA, it is estimated that 21 million U.S. adults (aged 18 and above) suffer from major depression. That works up to 8.4% of the adult population in the state.
Depression is mainly treated with psychotherapy and medications, such as monoamine oxidase inhibitors (MAOIs) and selective serotonin reuptake inhibitors (SSRIs). For people who don’t respond to these treatment methods (also called treatment-resistant depression), transcranial magnetic stimulation (TMS) is typically prescribed by medical providers. TMS therapy, which has been around since 1985, is currently used to treat a wide range of mental health and neurological disorders.
TMS Therapy
Are you or someone you know struggling with depression? Have you tried multiple treatments, but nothing seems to work? Transcranial Magnetic Stimulation (TMS) Therapy might be the solution you’re looking for.
Definition
Transcranial magnetic stimulation (TMS) is a non-invasive brain stimulation therapy that utilizes electromagnetic pulses to stimulate the brain, which may improve the symptoms of neurological and mental health conditions.

Because TMS involves repetitive electrical impulses, it is frequently referred to as repetitive transcranial magnetic stimulation (rTMS). When people undergo treatment for depression using TMS, an electromagnetic coil will be held against the scalp of their head. This coil emits magnetic pulses that activate nerve cells in the brain region involved in regulating mood and depression. Medical experts believe TMS stimulates the parts of the brain that become less active when someone has depression. Depending on the equipment and clinical protocol that is being employed, the length of time for each session can range anywhere from 20 to 50 minutes.
Effectiveness
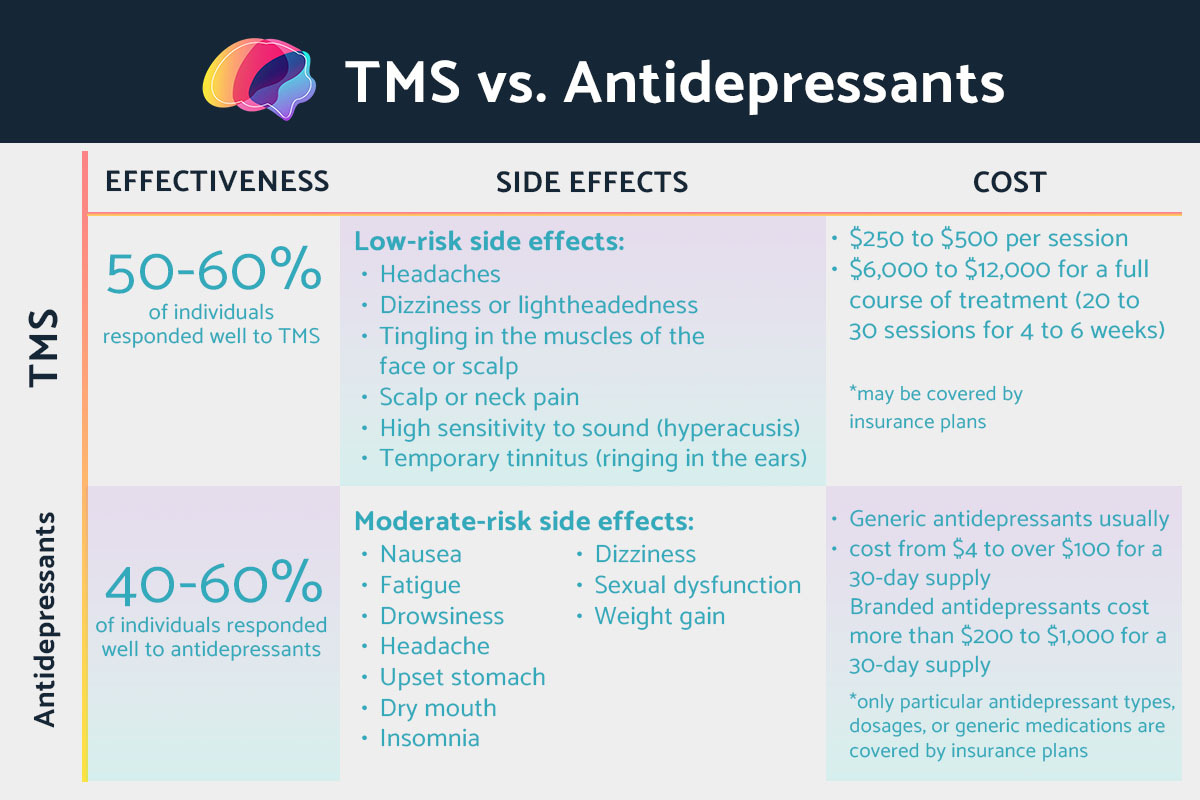
The treatment of depression using TMS appears to have a high success rate. There is a 50–60% range in terms of response rates for TMS. TMS is also steadily emerging as an effective tool in managing treatment-resistant depression. The vast majority of patients report that it is safe and that they tolerate it well.
TMS has also been shown to be safe and effective for pregnant and elderly patients. However, there is a need for additional research to determine the success rate for treating other medical issues, such as obsessive-compulsive disorder.
Side Effects
Transcranial magnetic stimulation is associated with a comparatively low risk of side effects and complications. Seizures are the most significant adverse reaction that can occur from TMS. However, instances of seizure are incredibly uncommon.

The following potential side effects are minor and disappear within a few minutes after treatment ends:
-
Headaches
-
Dizziness or lightheadedness
-
Tingling in the muscles of the face or scalp
-
Scalp discomfort or neck pain
-
High sensitivity to sound (hyperacusis)
-
Temporary tinnitus (ringing in the ears)
In most cases, the coil placement and the dose are only performed once. This takes place during the initial treatment. Measurements taken during the initial treatment are used to guide the position of the magnet during subsequent treatments.
Patients will put in their earplugs during treatment and relax in a chair while the magnetic coil is pressed against their heads. When the equipment is turned on, they will feel and hear fast tapping on the scalp. The pattern will consist of a rapid tapping followed by a break. They may feel pain or discomfort on the scalp while tapping but not during the breaks. Throughout the procedure, the patients are awake and aware. Depending on the stimulation pattern used, the treatment can take 20 minutes to complete.
After finishing treatment, they may be able to get back to their regular activities. In some cases, they may experience temporary headaches but are able to work and drive safely between treatments.
Standard care, such as medication and talk therapy, may be advised once a course of TMS treatment for major depressive disorder has been completed.
Thinking of making a change for the better? Call us now at (323) 792-2071 or message us from our contact page to find out more about how TMS therapy can support your mental health journey.
Cost and Insurance Coverage
The average cost of a single TMS treatment session is between $250 and $500. A full treatment course may cost $6,000 to $12,000 (20 to 30 sessions for 4 to 6 weeks). Depending on a person’s pre-existing medical condition, their health insurance company may provide coverage. They may be required to take four or more antidepressant medications before obtaining TMS coverage. They may also cover insurance if a person has a negative reaction to antidepressants. Typically, repeated TMS treatments are covered by insurance plans. People may call and check with their insurance provider whether or not they will cover the costs of TMS.
If you or a loved one are experiencing depressive symptoms, seek immediate medical attention. Lucid Wellness Center in Los Angeles provides a free initial consultation with a board-certified psychiatrist. Schedule your free consultation with us today!
Antidepressants
Definition
Antidepressants are a medication class that is prescribed to individuals suffering from depression. They restore the brain’s chemical imbalance by acting on the neurotransmitters. According to medical experts, neurotransmitters are responsible for the alterations in mood and behavior.

Most antidepressants come in tablet form. When recommended, a person will start taking them in the smallest dose likely to alleviate their symptoms effectively.
Antidepressant medications come in a few distinct categories:
-
Selective serotonin reuptake inhibitors (SSRIs). In many cases, doctors prescribe SSRIs as the first line of treatment. Compared to other antidepressants, these medications are preferred because of their lower risk of side effects and higher tolerability. SSRIs work by reducing the amount of serotonin that is taken in by the brain. As a result, communication between brain cells is facilitated, and individuals experience stable moods. Perhaps the most well-recognized SSRI is fluoxetine (Prozac). Citalopram (Cipramil), escitalopram (Cipralex), and sertraline (Lustral) are among other SSRIs available.
-
Serotonin-norepinephrine reuptake inhibitors (SNRIs). SNRIs are remarkably similar to SSRIs. SNRIs increase both serotonin and norepinephrine levels. These neurotransmitters are important in stabilizing mood. SNRIs include duloxetine (Cymbalta), levomilnacipran (Fetzima), and venlafaxine (Effexor XR).
-
Tricyclic antidepressants (TCAs). The levels of serotonin and norepinephrine absorbed by the brain are controlled TCAs, which reduce symptoms of anxiety and depression. Tricyclic antidepressants include nortriptyline (Pamelor), imipramine (Tofranil), and amitriptyline (Elavil).
-
Monoamine oxidase inhibitors (MAOIs). MAOIs work by inhibiting monoamine oxidase, an enzyme in the brain that aids in the breakdown of neurotransmitters like serotonin. This may result in a more stable mood and less anxiety. MAOIs include isocarboxazid (Marplan) and phenelzine (Nardil).
-
Atypical antidepressants. Atypical antidepressants are distinct from other types of antidepressants. Each of these drugs has its unique mechanism of action. This type of antidepressant includes bupropion (Wellbutrin XL), trazodone (Desyrel), and mirtazapine (Remeron).
Effectiveness
Antidepressants are helpful in treating depression. The Institute for Quality and Efficiency in Health Care reports that 40% to 60% of individuals, within six to eight weeks of beginning treatment with SSRIs or SNRIs, claimed to experience some improvements in their symptoms. However, not everyone has the same results as a certain antidepressant medication.
According to a study by Oxford University, one of the most effective yet least tolerated antidepressants was amitriptyline. On the other hand, Prozac— currently off-patent and known by its generic name, fluoxetine— was the least effective but most tolerated antidepressant.
Side Effects
The antidepressant’s side effects may be troublesome during the first few weeks, but they usually fade away once time has passed. Even if people experience negative side effects, they must keep taking their medication as prescribed.

The potential adverse effects of antidepressants vary widely depending on the drug’s class and the specific brand used. In general, antidepressants have the following common side effects:
-
Nausea
-
Increased blood pressure
-
Fatigue
-
Drowsiness
-
Headache
-
Upset stomach
-
Dry mouth
-
Insomnia
-
Dizziness
-
Blurred vision
-
Sexual dysfunction
-
Weight gain
These side effects tend to subside over time. If individuals experience adverse effects, it’s important for them to communicate with their primary care provider. They might suggest switching medications or adjusting their current dose.
Cost and Insurance Coverage
Antidepressants available in generic form are much more cost-effective than their brand-name counterparts despite having the same active components. Generic antidepressants usually cost from $4 to over $100 for a 30-day supply, while branded antidepressants cost more than $200 to $1,000 for a 30-day supply. Some insurance providers and Medicare pay for the cost of generic antidepressants. However, antidepressants may not always be fully covered by insurance or cover particular types, dosages, or generic medications.
At Lucid Wellness Center, we care for you above all else. Call us now at (323) 792-2071 to find out more about our services and how we can make a difference.
Which Treatment Should You Choose?
It is essential to discuss the various treatment options with a certified medical or mental health professional before settling on a course of action for treatment. This will allow individuals to better understand the range of options available.
Both antidepressant medication and transcranial magnetic stimulation (TMS) provide effective relief from the symptoms of depression. The first-line treatment for major depressive disorder often consists of medication (such as SSRIs or SNRIs) and psychotherapy. TMS therapy, on the other hand, can be helpful for those who haven’t found relief from medications or who are unable to tolerate them.
TMS is a non-invasive treatment option that has the potential to improve one’s quality of life and can be used individually or in conjunction with other therapies or medications. Patients who struggle with major depressive disorder may find this non-invasive procedure helpful.
If you’re struggling with mental health issues, it’s crucial to talk to a trained professional who can help weigh your options and select the best course of action given your unique situation.
Mood disorders like depression affect millions of individuals every year, but help is available for them. At Lucid Wellness Center in Los Angeles, we understand that everyone struggling with depression encounters unique challenges. Our compassionate medical support and evidence-based treatment approaches are aimed at enhancing each patient’s quality of life.
Conclusion
Major depressive disorder, often known as clinical depression, is a mental health disorder that can significantly influence a person’s capacity to lead a healthy and engaged life. Fortunately, a range of approaches might lessen or eliminate symptoms and achieve remission. Antidepressants and transcranial magnetic stimulation are two of the most effective treatments.
Antidepressants restore a healthy balance of brain chemicals, thus regulating mood and emotion. They come in various forms, each tailored to work with an individual set of neurotransmitters. While some people feel better after taking a single medication, others have to try several different medications before discovering one that works for them.
However, antidepressants don’t work for everyone. Sometimes the prescription has no impact, or the adverse effects are too much to bear. Many patients who have tried treatments for depression without success have found symptom relief through TMS.
TMS is effective for treating depression because it directly stimulates the regions of the brain. It effectively alters neural pathways and deeper brain structures, substantially improving depressive symptoms.
Seeing a mental health professional is recommended, as depression can only be diagnosed by a board-certified professional. Talk therapy, in which people learn to manage their thoughts and emotions, or a combination of TMS therapy and antidepressant medicines, is commonly prescribed by mental health specialists as a form of depression treatment.
Seek emergency services or medical attention if you or your loved one is suffering from major depressive disorder but do not have resources for treatment options yet. The sooner you get medical assistance, the sooner you or a loved one feel better and return to a sense of wholeness.
TMS therapy offered at Lucid Wellness Center in Los Angeles is deemed to be among the most effective treatments available for depression and a variety of other mental health conditions. Lucid Wellness Center has been at the forefront of developing innovative therapies like TMS to help clients rediscover hope and find the healing they’ve been seeking. Send us a message through our contact page today to learn more about our services.
Frequently Asked Questions
What is TMS Therapy?
How is TMS Therapy Different from Antidepressants?
Transcranial magnetic stimulation (TMS) is often administered for patients with depression who don’t respond to antidepressants. TMS and antidepressants are both effective for depression, but they vary in terms of method of administration, cost, and side effects.
Is One Treatment More Effective than the Other?
Is There a Risk of Side Effects with TMS Therapy and Antidepressants?
What are the Financial Costs Associated with Each Treatment?
TMS typically costs $250 to $500 per session or $6,000 to $12,000 per cycle (20 to 30 sessions for 4 to 6 weeks). Meanwhile, generic antidepressants cost from $4 to over $100 for a 30-day supply, and branded antidepressants cost more than $200 to $1,000 for a 30-day supply.
Does Insurance Cover TMS Therapy and Antidepressants?
Are There any Potential Lifestyle Changes that can Help with Depression Symptoms?
Stress can amplify the symptoms of depression, so it is helpful to manage it. Stress can be managed with regular exercise, a balanced diet, and adequate sleep. Yoga and meditation are some examples of mindfulness practices that can help people cope with stress.
Can Both Treatments be Used Together to Maximize Benefits and Minimize Side Effects?
Yes. In most cases, combining treatments is the most effective approach for depression. Some patients report that when TMS is combined with an oral antidepressant, they are better able to achieve full remission from depression. A psychiatrist may advise individuals to take antidepressants alongside TMS therapy based on their unique medical history and needs.
An individual may consult a psychiatrist to determine whether they require TMS and antidepressants.
Are There any Health Conditions or Medications that Might Interfere with Either Treatment Option?
How Often Do Individuals Need to Receive Treatments such as TMS Therapy in Order to Experience Lasting Results from It?
Are Individuals able to Switch Between Both Options if They Stop Working at Some Point in Their Journey Toward Feeling Better Overall?
NIMH. (2022). Major Depression. https://www.nimh.nih.gov/health/statistics/major-depression
Noohi, S., & Amirsalari, S. (2016). History, Studies and Specific Uses of Repetitive Transcranial Magnetic Stimulation (rTMS) in Treating Epilepsy. Iranian Journal of child neurology, 10(1), 1–8.
Harvard Medical School. (2020, October 27). Transcranial magnetic stimulation (TMS): Hope for stubborn depression. https://www.health.harvard.edu/blog/transcranial-magnetic-stimulation-for-depression-2018022313335#:~:text=Does%20TMS%20work%3F,their%20symptoms%20go%20away%20completely.
Chail, A., Saini, R. K., Bhat, P. S., Srivastava, K., & Chauhan, V. (2018). Transcranial magnetic stimulation: A review of its evolution and current applications. Industrial psychiatry journal, 27(2), 172–180. https://doi.org/10.4103/ipj.ipj_88_18
Somani, A., & Kar, S. K. (2019). Efficacy of repetitive transcranial magnetic stimulation in depression: the evidence thus far. General psychiatry, 32(4), e100074. https://doi.org/10.1136/gpsych-2019-100074
InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. Depression: How effective are antidepressants? [Updated 2020 Jun 18]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK361016/
The Guardian. (2018, February 21). The drugs do work: antidepressants are effective, study shows. https://www.theguardian.com/science/2018/feb/21/the-drugs-do-work-antidepressants-are-effective-study-shows

